Out of 5,000 daily deaths globally because of Tuberculosis, India accounts for 1,400. Two deaths occur every three minutes. It reports most number of cases, and this is when you don’t take into account the “missing million”, as they are called – those who go undiagnosed. India also has the largest number of cases of Multi-Drug Resistant TB (MDR).
“I have worked in both, the private and the government sector, and I can assure you that there is no way to reduce the huge burden of TB in India, until the two come together and work together via a care and referral system,” says Dr Vikas Oswal, a chest specialist at Sai Hospital in Dharavi. India has an estimated 2.3 million people currently living with TB.
Chasing Away TB in Dharavi, Asia’s Largest Slum
In a high-risk area like Dharavi in Mumbai, the cases of MDR TB are alarmingly high. In 300 square feet rooms, dozens of men and large families live and work together, with almost no ventilation up the narrow stairways in dark bylanes.
But it was the lack of a support system for local doctors to diagnose and follow up with hundreds of TB cases that led to this situation. Patients are often misdiagnosed, have the wrong dosage of the heavy medication, or simply drop out. This is the roadblock that PATH’s care-and-referral networking project aims to dissolve to tackle urban TB through: Private Provider Networking Interface (PPIA).
How To Fight TB: Step 1
PPIA allows local doctors like Dr Sushil Singh (AYUSH), in areas like Dharavi, to prescribe X-ray and sputum tests via a voucher program in cases they suspect are positive for TB. The patient then takes the voucher and heads to a nearby laboratory, also tied up with PATH.
- 01/03Dr Singh meets with at least 100 patients a day in his small two-room clinic. (Photo: Pallavi Prasad)

- 02/03Medicine cabinet of Dr Singh’s clinic. (Photo: Pallavi Prasad)

- 03/03The clinic’s pharmacy, for an estimation of scale. (Photo: Pallavi Prasad)

I get at least 10-15 positive cases of Tuberculosis each month, and that’s only in this area of Dharavi. There’s no awareness. If it’s present in their sputum and they spit, it’ll spread. Due to PATH, at least the financial and logistical burden of getting X-rays, tests and medicines is taken care of, and the patient’s course of medicines is also completed. Otherwise, they go to some informal medical practitioner who’ll treat them for the wrong thing, or to a GP in the private sector which doesn’t always follow guidelines when it comes to TB.Dr Sushil V Singh, AYUSH specialist in Dharavi
How to Fight TB: Step 2
In case of symptoms of positive cases, the doctor then refers the patient to a chest physician in a “hub hospital”, who provides specialised testing and care. Cost of all tests and first-line medicines are subsidised through vouchers issued by a centralised network, and issued via text messages. In MDR cases, the incidence is referred to the government.
How To Fight TB: Step 3
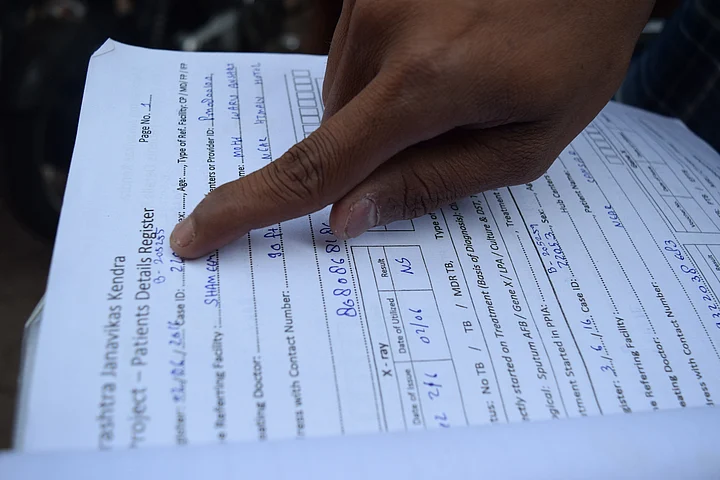
Reminders to eat medicines, follow-up for appointments, home visits and counsellors’ services are also made available via phone calls, and with the help of Non-Governmental Organisations such as the Maharashtra Janavikas Kendra (MJK).
The patient’s data also get uploaded on Nikshay, the government’s online portal for TB monitoring, thus helping in narrowing the gap between identified and notified cases.
- 01/03An MJK volunteer explains how patients are tracked for follow-up. Documentation is crucial to fight TB, especially with India accounting for 60% of the gap between incidence and reported cases. (Photo: Pallavi Prasad)

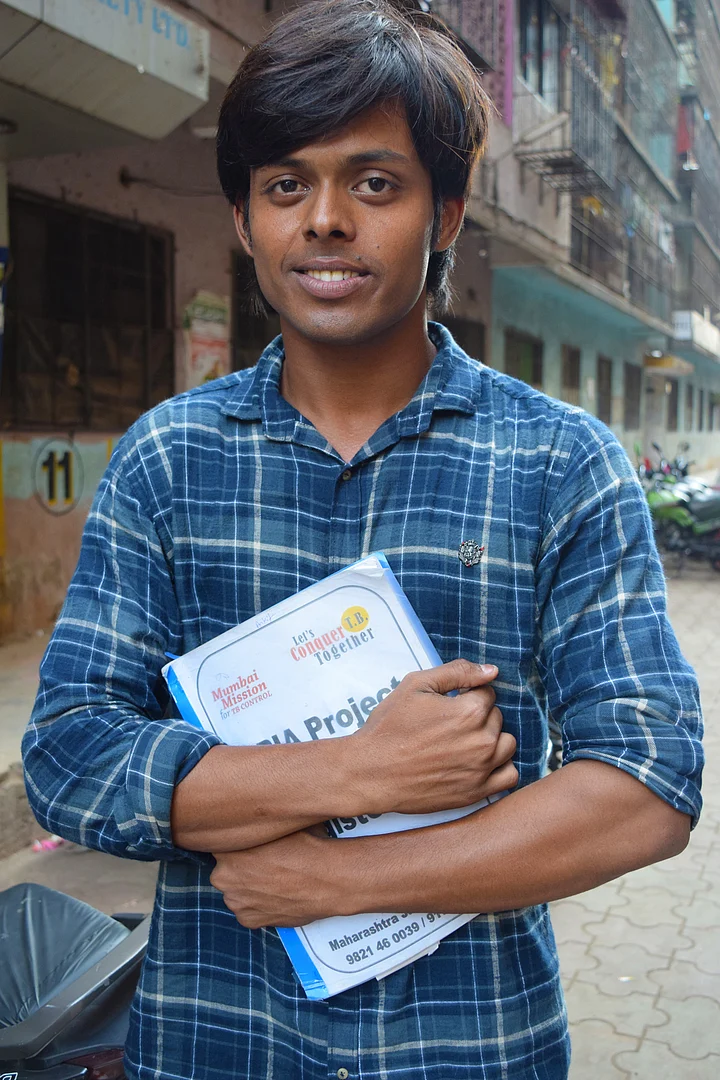
- 02/03A field worker from MJK explains how they are trained to go visit homes of patients who don’t show up for follow-up appointments and drug refills to encourage them to finish their treatments. (Photo: Pallavi Prasad)

- 03/03Sachi is the much-loved PATH coordinator for this area who knows the names of patients and each of their family members. (Photo: Pallavi Prasad)

A Survivor’s Tale
Meet Taibunnisa, a nearby resident in Dharavi, lives with her husband, who is the centre of her world, and three children, who are everything to her. After her family doctor dismissed her worries when her ten-day old cough wouldn’t get better with his prescription, she gathered courage and went to her hub’s centre for TB tests.
After her reports from Sai Hospital came back positive, field workers from MJK visited her house and advised to keep distance from her young children. She couldn’t imagine doing it; her husband refused, saying “we’ll all die together.”
“But I wanted to live; I didn’t want to die,” Taibunnisa narrates. And so, she lived away from her family for three months, took her medicines without missing a day, and went for all her appointments and counselling.
When my test reports came back positive for Tuberculosis, I was shaken. I went home and told my family and they started crying. He was thinking if something happened to me , the children’s lives would be over because he couldn’t handle it alone, and the name of TB itself was very scary. I knew nothing about TB, except that ‘it kills’. I thought there was nothing more dangerous than TB. I thought death was in front of me and my days were numbered.Taibunnisa, a TB survivor
Earlier, I was ashamed of telling people that I had TB, fearing they would distance themselves from me and treat me differently. But now, after getting a second chance at life, I want to tell people I had TB. So what? There’s a cure for it also! My doctor and people at PATH gave me so much encouragement to carry on with my nine-month treatment, otherwise I had lost all hope.Taibunnisa
(At The Quint, we question everything. Play an active role in shaping our journalism by becoming a member today.)