What happens when an epidemic goes out of control and becomes commonplace? What happens if the drugs that once saved lives stop working for you?
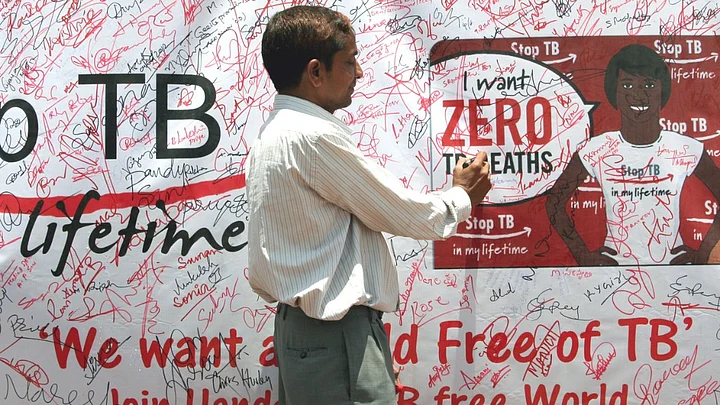
The Tuberculosis epidemic in India is one such example, where despite measures for control and treatment for the past 50 years in the country, disease rates soar and kill Indians by the hour.
It’s not that the public health system in the country hasn’t responded or that the strategies for TB control haven’t yielded results. It’s that the scale of the problem has escalated, with not enough focus on prevention of the disease.
Delayed detection of the disease and inappropriate treatment are the biggest issues. Lack of sanitation and overcrowded urban areas make disease transmission easier. Low awareness levels add to the woes. Low health infrastructure coverage in rural areas makes the treatment longer.
And then there’s the extra burden of drug resistance in TB – perhaps the single-biggest worry for public health experts.
Even as the health ministry pledges to eliminate Tuberculosis in India by 2025, what are the key issues in TB control and what is the way forward?
For World TB Day, we invite Professor Ramanan Laxminarayan for an expert commentary on the state of affairs of the TB epidemic in India.
Tuberculosis Epidemic in India
Tuberculosis (TB) is one of the top 10 causes of death globally. A quarter of all TB cases occur in India.
TB incidence in India in 2015 stands at 2.2 million cases out of a global incidence of 9.6 million, according to World Health Organization (WHO) estimates.
Every year, many new cases are added and unfortunately, many more go undetected. Under-reporting of TB cases has been one of the impediments for effective TB control in India.
In 2016, a study published in The Lancet found that India could have two times more TB cases than currently estimated. There’s an urgent need to strengthen disease surveillance to implement appropriate policies and interventions.
A bigger challenge the country is facing is the spread of multi-drug resistant TB (MDR-TB) and extensively drug resistant TB (XDR-TB). An estimated 71,000 drug-resistant TB cases were detected in 2014 .
In simple terms, MDR-TB is a form of TB in which patients do not respond to at least one of the main TB drugs. With XDR-TB, they are resistant to at least four of the core anti-TB drugs.
MDR-TB and XDR-TB are more difficult, expensive and take longer to treat using second-line anti-TB drugs. These drugs, in fact, have more side-effects than the first-line drugs.
While antibiotic resistance can arise as a result of inappropriate treatment or misuse of the drugs, these drug-resistant forms of infections are also passed on directly from one person to another.
For example, a recent study by the Center for Disease Dynamics, Economics & Policy (CDDEP), published in the International Journal of Tuberculosis and Lung Disease, has estimated that one urban TB case will infect an average of 12 people per year and remain infectious for about one year, while a rural case will infect an average of 4 people per year, but remain infectious for more than two years.
This indicates that while urban Indians may have better access to appropriate TB treatment, they may pass on the infection to more people than their rural counterparts.
Steps Taken to Improve TB Control
India has taken steps to improve TB control. In 2012, India became the first country to ban TB antibody tests, widely available in the private market, but which often misdiagnosed TB.
Misdiagnosis – either missing a TB diagnosis in someone who has the disease or diagnosing TB in someone who does not have it – is damaging.
Not treating someone with TB means a poorer outcome for that person, and continued risk of transmission to others. Patients who do not have TB and are misdiagnosed maybe put on powerful drugs, which can be toxic for the liver, kidneys and brain.
In the same year, India made TB a notifiable disease, making it mandatory for all government and private health facilities to record and report all cases to the national TB control program in India.
In 2015, the Indian government took strong steps to ensure that irrational drug combinations, including those for TB, were banned. Without this, the pharmaceutical companies were free to introduce newer drug combinations, easily evading the price ceilings set by the government to ensure accessibility of life saving drugs to all.
Still a Long Way To Go
Globally, a new anti-TB drug, Bedaquiline, is the first one to be approved (2012) in more than 40 years by the US Food and Drug Administration (FDA). The drug has been hailed as having the potential to dramatically improve MDR-TB treatment outcomes, preventing thousands of deaths.
But for a large number of TB patients in India who go to the private sector for treatment, cheaper drugs are the need of the hour.
In February this year, the WHO published a list of antibiotic-resistant "priority pathogens", to address the growing concern of antimicrobial resistance (AMR) but omitted TB from the list, leading to controversy and indicating the low priority often given to TB control programs.
The TB epidemic was declared a global health emergency in the early 90s but even two decades later, it continues to take thousands of lives each year. Urgent and aggressive measures need to be implemented for both prevention and treatment if India wants to fight the epidemic.
(Professor Ramanan Laxminarayan is an infectious diseases expert. He is the Director at Center For Disease Dynamics, Economics & Policy.)
(For World Tuberculosis Day, FIT is posting a series of articles to raise awareness about the disease, including actions to address stigma, discrimination, marginalisation and overcome barriers to access care.)
(At The Quint, we question everything. Play an active role in shaping our journalism by becoming a member today.)