Having practiced critical care for almost 30 years in both first world and third world countries I continue to be amazed by how little I know or more importantly how dynamic critical care is. Already, before the coronavirus, ICU beds are our most resource-intensive place to provide care in any hospital. The use of them is guarded very, very carefully—most intensivists spend a lot of their day figuring out who needs one the most, when they can get it, and when they can get someone else out to a regular floor. And still, ICU beds are often full. Even though general occupancy may suggest otherwise, I’ve rarely known an ICU to have beds freely available. Even if the actual bed is empty, there is often not enough staff—usually nursing—to provide care, and so that bed cannot really be used.
A Ventilator Does Not Make an ICU Bed
As the corona pandemic spreads there are certain facts. 80% of affected patients will have a milder form of flu which can be treated at home, 20% need some form of hospital care and about 5-8% will require intensive care. The confounding factors will include age, co morbid or other diseases and the current immune state.
There has been a passionate following in the general media about the number of available ventilators and the new enthusiasm to make one regardless of complexity, function and quality. There is a generalist belief that as soon as we crank up the numbers we will be able to handle the loads of projected patients- just get these machines into the hospitals!
Unfortunately nothing is simple in this analogy and reminds me of cranking up car production without producing enough drivers.
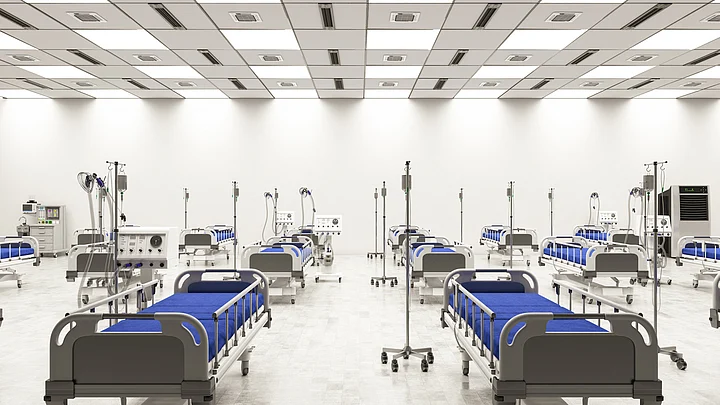
We only have 29,000 ICU beds in the country and quite frankly most are of dubious quality. There are multiple reasons for the above statement but the most important is that it costs an enormous amount of money to set one up.
In India a comprehensive ICU bed would cost 1 crore per bed and almost 1 million USD in the West.
In India a comprehensive ICU bed would cost 1 crore per bed and almost 1 million USD in the West.
The primary issue is the specific building design, infection free rooms and very expensive monitoring equipment with things like specialised beds, pumps for iv fluids, special lighting, air handling units etc. These beds need to then be serviced by technical support services such as TOP notch laboratory or diagnostics, radiology, blood bank and therapists.
In addition, the non clinical services are again specialised in all respects whether it is sterilisation of equipment, laundry, house keeping and even different biomedical waste.
How Do We Reduce the Burden on ICU Beds?
What should we do? Break it up into short term and longer term imperatives.
First use the power of telemedicine to get virtual expertise into these hospitals by having multiple command centers with trained doctors guiding those not trained. We don’t need sophisticated equipment but a simple audio visual will do- after all mobiles are now ubiquitous in all part of our country.
Quickly standardised protocols and put them on line for mass use.
Ensure supply of essential drugs and consumables.
Enable simple diagnostics like X-ray machines and ultrasounds.
Let’s accept that this is not ideal but a war demands speed and not perfection.
The above scenario clearly indicates that we will never have enough ICU resources if the numbers begin to soar and community transmission becomes endemic. So what can save us now is the break the circuit of transmission. The country cannot stay in lock down forever but what can become ingrained is personal hygiene, dissuade aerosol transmission by using a barrier, isolating patients, mass antibody testing to identify people who have had the infection and have demonstrated an immune response and finally identification of hot spots to clamp down on further disease using all of the above.
This may ensure that we will get through this without the current fixation of just delivering ventilators.
(With over 20 years of clinical, investment and operational experience in the healthcare sector, Dr Amit Varma brings with him a domain expertise that links all facets of healthcare. He is a reputed physician with diverse healthcare management leadership roles and has headed numerous companies)
(At The Quint, we question everything. Play an active role in shaping our journalism by becoming a member today.)