The Government of India announced its plan to eliminate tuberculosis (TB) by 2025, five years ahead of the previous target of 2030.
The declaration, though encouraging, is extremely ambitious. I say this considering the magnitude of the problem – according to the latest figures available from the WHO, India accounts for 27 percent of the world’s 10.4 million new TB cases and 29 percent of the 1.8 million TB deaths globally.
This begets the question of how India can translate this vision to actuality. Here are ten issues to prioritise if we are to bridge the gap between ambition and reality.
1. Invest Resources
First and foremost, India needs to prioritise and invest adequately, commensurate to the scale of India’s TB epidemic. There was anticipation of a tripling of the budget for the period 2012-2017, but this did not happen.
In February 2017, the Revised National Tuberculosis Control Program (RNTCP) published a new National Strategic Plan (NSP) for TB Elimination 2017-25 and requested for a budget of Rs 16,649 crore (USD 2,485 million), an exponential rise from the last NSP (2012-17), which was not even fully funded.
In the 2017 Union Budget, there is some indication that TB will get a higher allocation (of Rs 87 crore over a year to 2017-18), but a recent analysis by IndiaSpend suggests a drop of Rs 13 crore over 2016-17.
2. Address Social Determinants
India must seriously tackle the social determinants of TB, especially malnutrition and tobacco smoking, which have established linkages with TB deaths.
Inter-sectoral collaboration between various ministries, agencies and civil society organisations, therefore, would be crucial. Addressing these factors will not only lower the risk of TB, but other diseases as well.
3. Improve Access to Diagnostics
Our existing public health system depends heavily on sputum microscopy which has lower detection rates (~55%).
Advanced diagnostic tools that can detect drug resistance in a matter of two hours need to be used to universalise drug susceptibility testing (DST) to detect drug resistance at the very initial stages.
The government will need to acknowledge that such diagnostics are essential to care and must ensure they are affordable and easily accessible.
4. Improve Access to Treatment
India needs to expedite the scale-up of the globally adopted daily drug regimen instead of the intermittent regimen (thrice a week).
The delayed introduction of the daily regimen and petitions by activists has prompted the Supreme Court of India to direct the government to switch from intermittent therapy to an internationally accepted daily regimen by October 2017.
Furthermore, our health system’s regulation and operations must be properly adjusted to roll out newer medication and more effective regimens in the future without delays.
5. Integrate Supportive Schemes & Services
Supportive services and social welfare programs need to be extended to communities affected by TB.
Schemes for particularly vulnerable groups that focus on socio-economic protection through direct benefit transfers, linking existing subsidies, providing additional nutrition and transport can address the devastating socio-economic impact of the disease.
Additionally without appropriate counselling services (eg: testing/treating co-morbidities, pre-treatment and treatment management, and psychological) to support affected communities through their illness we run the risk of ignoring barriers that prevent treatment completion and cure.
6. Engage with the Private Sector
The Indian government needs to engage more meaningfully with the private sector to ensure all patients are provided standardised treatment at affordable costs.
Studies show complicated, long, care seeking pathways, widespread mismanagement, and poor quality of care in the private sector.
Private Provider Interface Agencies programmes in Mehsana, Mumbai and Patna, have shown that notifications from the private sector can be dramatically increased, with improvements in quality and patient outcomes.
After a close assessment of the projects, it is imperative similar projects are expanded to other high-burden districts. At the very least, the government should ensure that private providers fulfill their requirement to notify all TB cases to the RNTCP.
7. Empower Communities
We need to empower affected communities by strengthening the TB community network (patients, survivors, civil society) and ensuring coordination with the TB programme.
We’ve seen in the past how crucial it is to involve communities to help tackle the stigma and discrimination associated with disease, as well as encourage accountability and responsiveness of the system.
8. Increase Awareness
The lack of awareness about the disease has been an obstacle for effective TB prevention and control in the past.
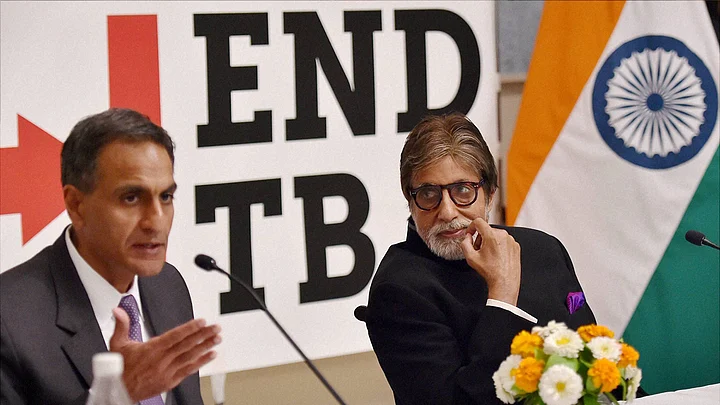
Recognising that awareness is the first step to behaviour change, awareness campaigns like the Amitabh Bachchan one, must be extensively disseminated to reach every nook and corner of the country.
9. Support Research
India must invest heavily in research and surveillance. Research must be directed toward the development of new point-of-care and accurate diagnostic tools, shorter drug regimens and an effective vaccine for children and adults.
Better surveillance will require periodic prevalence surveys, nationwide drug-resistance surveillance, improved public health informatics, better tracking of TB deaths, and implementation science to identify and treat missing TB patients.
The creation of the India TB Research and Development Corporation in November 2016 is a welcome move to encourage TB research, but it will require partnerships as well as sustainable funding.
10. Lead by Example
Finally, India needs to show sustained commitment from the political leadership toward the disease’s elimination and must consider it as a national emergency.
India stands at the cusp of great things and can be a global leader of this movement if we rise to the occasion. The National Health Policy and proposed increase in GDP spend on health to 2.5 percent is a major step in the right direction, and this we hope will allow for the new NSP to be fully funded and implemented.
(Dr Madhukar Pai is the Director of McGill Global Health Programs, and Associate Director of the McGill International TB Centre.)
(This piece was published on 10th April 2017 and is being re-published from FIT’s archives to mark World TB Day on 24 March.)
(At The Quint, we question everything. Play an active role in shaping our journalism by becoming a member today.)